Adenoid hypertrophy, or enlarged adenoids, is a common condition where the lymphatic tissue at the back of the nose becomes swollen, often leading to nasal obstruction, recurrent infections, and sleep disturbances. While most prevalent in children—affecting an estimated 34.5% of the pediatric population—it can also occur in adults, sometimes signaling other health concerns.
This condition sits at the intersection of immunology and obstructive sleep medicine. For parents and patients, understanding adenoid hypertrophy is key to recognizing symptoms early and seeking appropriate treatment to prevent complications like hearing loss, speech delays, or sleep apnea.
Understanding the Adenoids: Your First Line of Defense
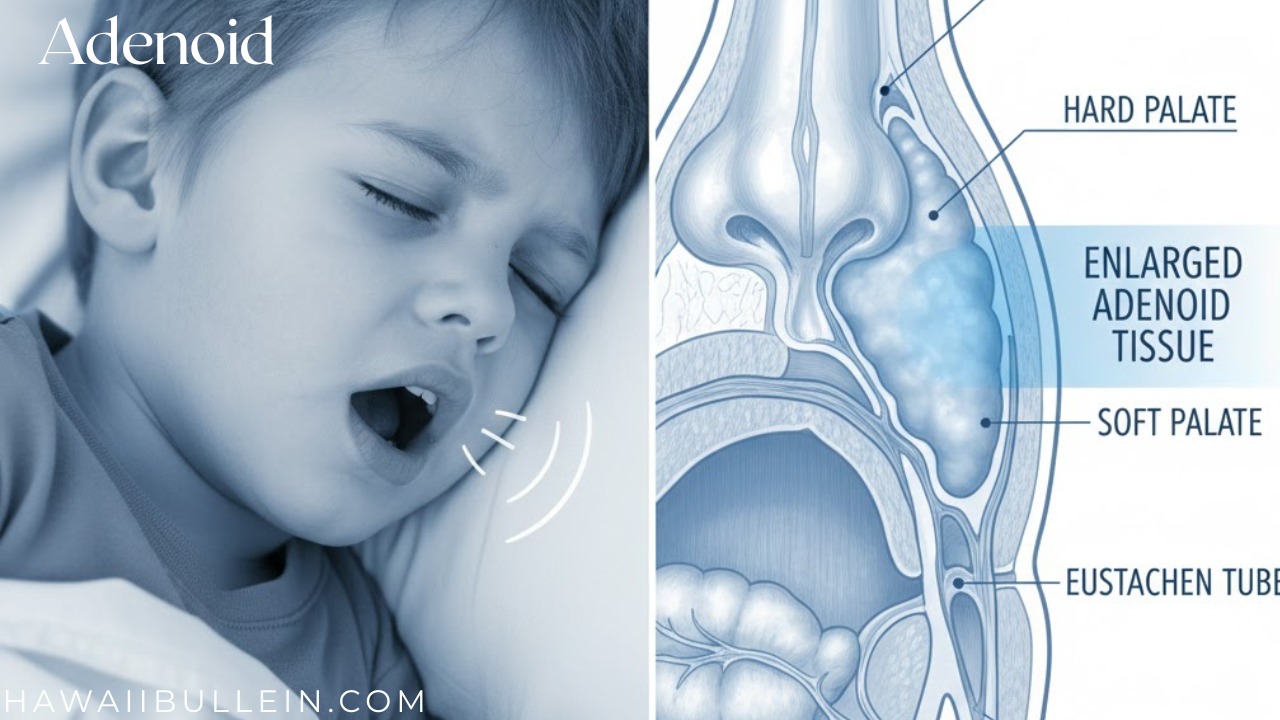
The adenoids are a single mass of lymphoepithelial tissue located high in the throat, behind the nose and the roof of the mouth (soft palate). You cannot see them by looking in the mouth like you can the tonsils. Together with the tonsils and other tissue, they form Waldeyer’s ring, a protective circle of immune tissue at the gateway to your respiratory and digestive tracts.
Their primary job is to trap bacteria and viruses you breathe in, helping the body build immunity, especially during early childhood. Their location makes them strategic defenders, but also vulnerable to becoming chronically infected or swollen.
Why Do Adenoids Become Enlarged?
Enlargement can stem from infectious and non-infectious causes:
-
Infections: Repeated or chronic battles with viruses (like adenovirus, rhinovirus, or EBV) or bacteria (such as Streptococcus or Haemophilus influenzae) can cause the tissue to remain in a perpetually enlarged, inflamed state.
-
Allergies: Chronic exposure to allergens can lead to persistent inflammation and swelling of the adenoid tissue.
-
Environmental Irritants: Exposure to cigarette smoke is a recognized contributor.
-
Physiological Growth: In many children, adenoids enlarge naturally during early childhood, peak around ages 6-7, and then typically atrophy and regress during adolescence.
In adults, where adenoid tissue is usually insignificant, new hypertrophy is unusual and should be investigated, as it can be associated with conditions like HIV infection, lymphoma, or sino-nasal malignancy.
Recognizing the Symptoms: From Snoring to “Adenoid Facies”
Symptoms arise from the physical obstruction of two key passages: the nasal airway (choanae) and the Eustachian tubes, which connect to the ears.
The following table categorizes the common symptoms and their direct causes:
| Symptom Category | Common Symptoms | Direct Cause of Symptom |
|---|---|---|
| Nasal Obstruction | Chronic mouth breathing, nasal congestion, hyponasal voice (“stuffed nose” sound), snoring | Blockage of the nasal airway by enlarged tissue |
| Ear Complications | Recurrent ear infections, persistent middle ear fluid (effusion), muffled hearing, ear pain | Blockage of the Eustachian tube opening |
| Sleep & Breathing | Restless sleep, sleep-disordered breathing, obstructive sleep apnea (pauses in breathing) | Partial or complete airway obstruction during sleep |
| Chronic Infection | Persistent runny nose, post-nasal drip, frequent sinus infections | Adenoids acting as a reservoir for bacteria |
| Facial Development | Adenoid facies: elongated face, high-arched palate, dental malocclusion | Long-term mouth breathing altering facial bone growth |
Why You Shouldn’t Ignore the Signs
Left untreated, the complications extend beyond a stuffy nose. Conductive hearing loss from chronic fluid can lead to speech and language delays and learning difficulties. Sleep apnea deprives the brain and body of oxygen, potentially leading to behavioral problems (like ADHD-like symptoms), bedwetting, poor academic performance, and in severe cases, pulmonary hypertension.
Diagnosis: How Doctors Evaluate Enlarged Adenoids
Diagnosis typically begins with a thorough history and physical exam. An ear, nose, and throat (ENT) specialist will look for the hallmark signs.
To directly visualize the adenoids—which can’t be seen with a standard throat exam—doctors use one of two main methods:
-
Flexible Nasopharyngoscopy: A thin, flexible scope with a camera is gently passed through the nose. This is considered a gold standard as it provides a direct, real-time view of the adenoid size and obstruction without radiation.
-
Lateral Neck X-Ray: A side-view X-ray can show the silhouette of the adenoids against the airway. While useful, especially for uncooperative children, it involves exposure to radiation.
Additional tests like sleep studies (polysomnography) may be recommended to quantify sleep apnea, or audiometry to assess hearing loss from ear fluid.
Treatment Pathways: From Medication to Surgery
Not all enlarged adenoids require surgery. The treatment path depends on the cause, severity, and impact on the child’s health.
Medical Management
For cases caused by infection or inflammation, initial treatment often involves:
-
Antibiotics: Used for acute or chronic bacterial infections.
-
Nasal Corticosteroid Sprays: Medications like fluticasone may help reduce adenoid size, particularly when allergies are a factor. However, benefits require consistent long-term use.
-
Allergy Management: Treating underlying allergies with antihistamines or avoidance can reduce inflammation.
Surgical Intervention: Adenoidectomy
When medical management fails or symptoms are severe, an adenoidectomy—surgical removal of the adenoids—is recommended. It is one of the most common childhood surgeries.
Common reasons for recommending adenoidectomy include:
-
Obstructive Sleep Apnea or significant sleep-disordered breathing.
-
Chronic or Recurrent Ear/Sinus Infections: Such as three ear infections in six months, or chronic sinusitis unresponsive to antibiotics.
-
Persistent Nasal Obstruction causing speech changes, dental issues, or adenoid facies.
-
Chronic Middle Ear Fluid with hearing loss.
The surgery is performed under general anesthesia and takes about 20 to 30 minutes. The surgeon works through the patient’s mouth, meaning there are no external scars. Various tools like curettes, suction electrocautery, or coblators are used to remove the obstructive tissue.
A critical preoperative check is for a submucosal cleft palate. Removing adenoids in a child with this undiagnosed condition can lead to severe speech problems, so surgeons must assess for it carefully.
Recovery and Prognosis
Recovery is usually swift. Most children go home the same day. For 1 to 2 weeks post-surgery, they may experience sore throat, earache, bad breath, stuffy nose, and a low-grade fever.
Care at home involves:
-
Hydration and Soft Foods: Encourage cool fluids, popsicles, soft foods (like pudding, mashed potatoes), and avoid crunchy, spicy, or acidic foods.
-
Pain Management: Over-the-counter pain relievers like acetaminophen or ibuprofen are typically sufficient.
-
Rest: Most children can return to school or daycare in 3-7 days.
The benefits are significant and long-lasting. Adenoidectomy improves sleep apnea symptoms in up to 85% of cases. It also dramatically reduces the frequency of ear and sinus infections. Importantly, removing the adenoids does not weaken a child’s immune system, which is highly adaptable and has many other tissues to perform immune functions.
Risks are rare but include bleeding (in about 0.1% of cases), infection, anesthesia reactions, and very rarely, regrowth of tissue or changes in voice quality.
A Guide for Parents and Patients
If you suspect adenoid hypertrophy, the first step is consulting a primary care physician or pediatrician, who can provide an initial assessment and refer you to an ENT specialist if needed.
Do not dismiss persistent snoring in children as normal. It is a primary warning sign of potential airway obstruction that warrants evaluation.
Keep a log of symptoms: note the frequency of ear infections, nights of loud snoring, observed pauses in breathing during sleep, and days of mouth breathing. This information is invaluable for your doctor.